-
- We acquired a massive federal dataset to analyze California’s nearly 1,200 “skilled nursing facilities” and found startling rates of patients with serious mental illness
- California might be violating the Americans with Disabilities Act
- We mapped nursing homes across the state based on percentage of residents diagnosed with a serious mental illness
- At the same time, we found that the state lacks a full accounting of nursing home residents with serious mental illness
- Few nursing homes are certified as “special treatment programs” — a designation indicating they have the skills and training to care for people with serious mental illness
- Citations fall short — effectively acting as slaps on the wrist for serious violations
- Questions remain about whether Gov. Newsom’s mental health plan will address the needs for suitable housing and services
Hyde Park Healthcare Center is a one-story building with a pink stucco and flagstone facade about 10 miles from downtown L.A. Seen from the street, it’s just another unassuming nursing home.
But inside, “It’s a sanitarium,” said Travell Jackson, a nurse with two decades of experience who worked at the facility in 2022. On any given day, she said, there were “patients running around, screaming, yelling, disrobing, defecating in the hallways, on themselves.”
Last year, 7 in 10 residents at Hyde Park had a serious mental illness — defined as schizophrenia, bipolar disorder, or psychotic disorder — according to an investigation by LAist, APM Research Lab and The California Newsroom.
Our investigation found that in 2022, hundreds of nursing homes across California — facilities that typically help people rehabilitate after surgery or provide round-the-clock care for the elderly or physically disabled — admitted and housed thousands of people with serious mental illness, often for a year or longer.
Nearly 100 of these nursing homes filled more than half of their beds with residents who have a serious mental illness; at some facilities, nearly every resident had a serious mental illness.
Our analysis also shows that the percentage of residents in California nursing homes who have a serious mental illness has been increasing over the past decade.
Experts say that keeping so many people with serious mental illness in nursing homes — rather than in community settings with appropriate services — amounts to “back door institutionalization” and “warehousing,” similar to what has happened in California’s prisons and jails for decades.

The consequences — documented in state records — have been horrific. Without proper supervision, residents with serious mental illness have slipped out of nursing homes and gone missing for weeks, and been released with little regard for their needs. Just a few examples:
- A 68-year-old woman with schizophrenia was found face down and barely alive in the rain by a passerby, 12 miles from her nursing home and a day after she wandered off. She died of hypothermia.
- A 46-year-old with schizoaffective disorder who’d recently attempted suicide walked out of a nursing home and jumped from an overpass onto the 101 freeway after hearing his dead father’s voice telling him to join him. He broke multiple bones, damaged organs and had to have a kidney removed.
- Another man with schizoaffective disorder who needed antipsychotic medication was released without a safe transition plan to an unlicensed group home, where he wound up eating his own feces; he died of sepsis.
Beyond the shocking anecdotes, experts say the failure of local and state governments to provide community-based care for people with serious mental illness could be a violation of the Americans with Disabilities Act.
We shouldn’t have this many people [with serious mental illness] living in institutions for months or years.
“It’s appalling,” said Eve Hill, a former deputy assistant attorney general with the U.S. Department of Justice’s Civil Rights Division, who also spent 30 years as a disability rights lawyer. “It’s very disappointing that this is still happening in spite of all the barriers we’ve tried to put up to prevent it from happening.”
Lawyers and academics also say that by allowing so many people with serious mental illness into nursing homes, the state of California could be violating a federal Medicaid law meant to prevent the institutionalization of people with psychiatric disabilities.
Our analysis also shows that the practice of housing people with serious mental illness in nursing homes brings down the average age of residents. And that has ripple effects. Nurses we spoke with said that being responsible for younger, more able-bodied residents makes it difficult to provide safe, quality care to older and less mobile people they were trained to help.
-
Nearly a year ago, we began the process of requesting and analyzing complicated federal data to examine our starting question: How many people with serious mental illness are residents in California nursing homes?
-
What we found was astonishing not just to us, but to lawyers and other experts steeped in nursing home and mental health policy.
-
Keep LAist journalism free for all with a donation today.
“That may not be the best compatibility,” said Rachel Tate, who heads L.A. County’s ombudsman’s office for long-term care. “That can be gravely concerning for a multitude of reasons.”
Speaking more broadly about the number of people with serious mental illness who are in nursing homes for extended periods, she said, “We as a society have failed them because there isn't necessarily a better option at this moment. Where else do you go?” Nursing homes, Tate added, have become “de facto mental health centers — but they don’t have the specialized training.”

Our shocking findings and the data behind them
We analyzed federal data for California’s 1,146 “skilled nursing facilities,” known commonly as nursing homes, which federal code says are “not primarily for the care and treatment of mental diseases.” None of these nursing homes are certified by the state as “special treatment programs” for psychiatric patients.
We found that in 2022:
- Nearly 22,000 nursing home residents had a serious mental illness; that’s 25% of all nursing home residents in California.
- Nearly 1 in 3 residents who’d been in a California nursing home for over a year had a serious mental illness.
- Almost 100 California nursing homes filled at least half their beds with people who had a serious mental illness; in several facilities, at least 8 in 10 residents had a serious mental illness.
- In 2022, nursing home residents with serious mental illness had spent nine months longer in their facility than those without serious mental illness.
- Less than 1% of long-term nursing home residents with serious mental illness received any psychotherapy in the week leading up to their annual assessments.
- Nearly one-third of residents in L.A. County nursing homes had a serious mental illness — the highest rate of any county in California.
We brought these findings to the California Department of Public Health, which handles licensing for nursing homes, and the Department of Health Care Services, which helps oversee community mental health care, for comment.
Responding jointly, the agencies asked us for the source of our data, which we provided. They followed up with findings from their own “initial analysis,” and concluded that the number of nursing home residents with serious mental illness is “likely lower than asserted” by our investigation. However, their analysis relied on a different dataset that covers a narrower population of nursing home residents than ours.
The agencies also noted that the presence of mental illness does not negate the potential need for skilled nursing care for people experiencing a range of conditions, from “advanced wound care” to “monitoring and management of chronic health conditions” such as diabetes to “dementia requiring safety monitoring (fall avoidance, wandering behavior mitigation).”
“It is important that individuals who are experiencing [serious mental illness] can access [nursing home] care when needed,” they wrote.
A possible violation of the Americans with Disabilities Act
We also brought our findings to leading academics, advocates and attorneys who specialize in nursing home policy and disability rights. Several of these experts told us that California could be violating Olmstead v. L.C., a landmark U.S. Supreme Court decision stemming from the Americans with Disabilities Act. Issued in 1999, the ruling says that state and local governments need to offer community services to people with disabilities so they aren’t unnecessarily institutionalized and segregated from the rest of society.
“Nursing homes generally are not the right setting for people with serious mental illness,” said Kevin Martone, a former New Jersey mental health commissioner who is now executive director at the Technical Assistance Collaborative, a nonprofit that works with states on mental health policy and Olmstead compliance. “People can generally be served in community-based settings with the right types of supports,” such as housing, case management and mental health services, he said.
Many states and local governments have come up short, including California and L.A. County, which for years have struggled with limited resources for community services along with an affordable housing crisis. As a result, people with serious mental illness and nowhere else to turn have ended up in institutions like hospitals, jails or nursing homes.
“If there’s nowhere to bring them into [the] community, then they’re stuck in the institutions,” said Jonathan Sherin, M.D., former director of L.A. County’s Department of Mental Health.
Sherin said people with serious mental illness often wind up in hospitals because they have co-occurring medical issues as they age, and don’t get great medical care to begin with. But when their hospital stay is up, their options are limited.
“If there was enough housing and enough support in [the] community,” he said, “we wouldn't be jamming up the streets, the jails, and things like [nursing homes].”
Our data found that 90% of California nursing home residents with serious mental illness came straight from hospitals.
[The state] should be investigating, because [nursing homes] certainly shouldn't have that large of a population unless they’re a special treatment facility.
Travell Jackson, the nurse who worked at Hyde Park Healthcare Center, said many new arrivals were unhoused. “People didn't have clothing, people didn’t have shoes,” she told us. “I'd ask them, ‘How did you end up here? Where’s your family?’ Some were just too far in their mental illness to give me a straight answer. It’s just sad.”

According to Tate, the L.A. County ombudsman, there’s a name for the most vulnerable people with serious mental illness — those with no reliable caretakers, no official conservator, no legal representation or ability to self-advocate — who end up in nursing homes as an alternative to the streets. They’re called the “unbefriended.”
“They don’t have the ability to protect themselves really, and they don’t have anybody to stand up and do it for them,” she said, “so they can sometimes get shipped and moved around.”

Tony Chicotel, senior attorney at California Advocates for Nursing Home Reform, put the problem in even starker terms. “For most residents with a serious mental illness, the nursing homes just serve as a warehouse — keeping them alive, keeping them fed and sheltered and out of the streets and out of people’s way,” he said. “We’re not accomplishing all that was hoped for with the Olmstead decision and the passage of the Americans with Disabilities Act.”
To stop states and local governments from segregating people with mental illness, the U.S. Department of Justice regularly investigates possible Olmstead and ADA violations. In 2018, the DOJ sued the state of Louisiana for the alleged segregation of residents with serious mental illness in nursing homes. The rate of serious mental illness in nursing homes in Louisiana was nearly identical to what we found in California
in 2022.
Map: How nursing homes compare
The DOJ declined to comment on our findings.
We presented experts’ concerns about a possible Olmstead violation to the California Department of Health Care Services and the California Department of Public Health. In their joint email, they wrote: “DHCS and CDPH perform several functions aimed at protecting the rights of Californians with disabilities to receive services in the least restrictive setting.”
Experts agree that people with serious mental illness should be able to get other types of care at nursing homes. But they say frequent and long-term stays look a lot like institutionalization — and a civil rights violation. “We shouldn’t have this many people [with serious mental illness] living in institutions for months or years,” said Lewis Bossing, senior attorney at the Bazelon Center for Mental Health Law, who has has been part of several lawsuits against government entities related to the Olmstead decision. California’s high rate of residents with serious mental illness in nursing homes, he said, “seems to be a failure of a system, a failure of any effort to rebalance a system — and an Olmstead problem.”

California lacks a full accounting of residents with serious mental illness
The California Department of Public Health told us it doesn’t keep track of all nursing home residents with serious mental illness.
The Department of Health Care Services, the other state agency in charge of mental health care, told us it keeps track of people with serious mental illness who have been through a federally mandated pre-admission screening process that’s supposed to steer residents with mental illness toward community services when appropriate. Yet our investigation found approximately 5,000 long-term residents with serious mental illness who in 2022 were not identified as such through the screening process.
“They’re looking the other way. They're just ignoring the problem,” said Charlene Harrington, professor emeritus of sociology and nursing at the University of California, San Francisco.
“It’s negligence,” said Kim Swain, former senior counsel at Disability Rights California, a nonprofit that has brought major disability rights lawsuits against local governments and the state. “No one’s paying attention to something that is having dire consequences.”
The pre-admission screening process has been so flawed that the state was deemed out of compliance by the federal government in 2015, at which point the feds compelled the state to create a corrective action plan. It wasn’t until June of this year, just weeks before the state’s deadline, that the feds gave California its stamp of approval.
Experts say the state’s failure to keep a complete count of the number of nursing home residents with serious mental illness could put them in violation of federal Medicaid requirements. That’s because the feds set a threshold for how many people a facility is allowed to accept because of their mental illness. Once nursing homes exceed that limit — 50% — they cannot get federal Medicaid funding for many residents. The state is responsible for identifying those facilities.
Swain said the state has little incentive to know which nursing homes have too many residents with serious mental illness. “Their Medicaid dollars would get yanked,” she said. “It would be chaos.”
In response to our findings and criticism from experts, the departments of Health Care Services and Public Health wrote, jointly: “We dispute the implication that DHCS and CDPH have little or no information” about nursing home patients with serious mental illness. The agencies explained that “both departments review extensive individual, patient-level data that includes diagnoses and service needs” as required, but said they “do not routinely perform data analytics for the express purpose of ‘counting’ or ‘tracking.’”
Toby Ewing thinks they should. He’s the executive director of the state’s Mental Health Services Oversight and Accountability Commission, which reviews how mental health services funds are spent. When we showed him our findings, Ewing told us, “You’ve done more work on this probably than the state of California has done.”
“It’s clear that we don’t have the data infrastructure that we need in order to better understand these trends as they’re happening,” Ewing said, “so that we can get in front of these challenges and really understand how we can intervene so that we don’t have inappropriate placements.”

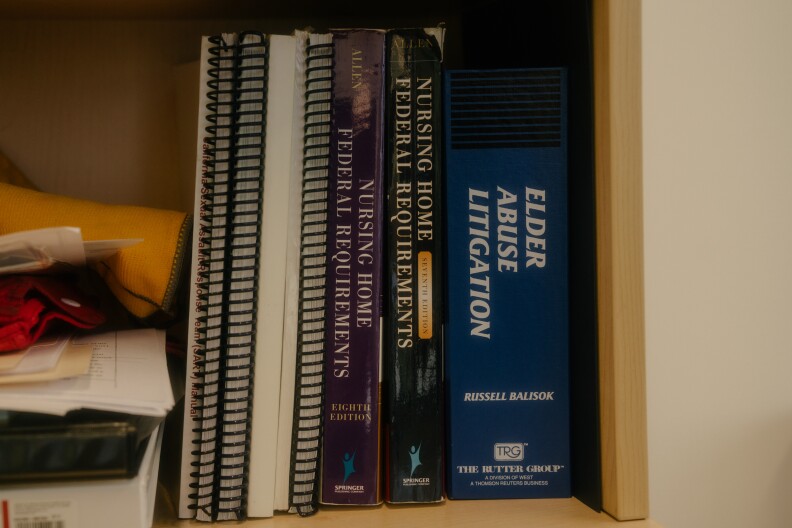
Few nursing homes are certified as special treatment programs
There’s a special category of nursing homes meant for patients with serious mental illness who aren’t ready to live on their own in the community: a “special treatment program,” or STP.
Under state requirements, STPs must have specially trained staff and therapeutic services that either help prepare patients for a more independent life, or prevent them from becoming less functional.
But only 31 of California’s nearly 1,200 nursing homes have STP certification, according to CDPH’s database.
One reason for the small number of facilities has to do with money. For starters, counties receive a limited amount of state dollars to put toward STPs, said Connie Draxler, acting chief deputy director of L.A. County’s Department of Mental Health. “There’s only so many dollars available,” she said. “So funding is an issue.”
And there’s another financial complication: Generally speaking, STP facilities that fill at least half their beds with seriously mentally ill patients can’t get federal funding.
According to [one citation], a resident with schizophrenia “elope[d] from the facility undetected” and was missing for 23 consecutive days before being found 18 miles away in a vegetative state with blunt-force head trauma.
On top of that, said Draxler, there’s the challenge of finding space and getting buy-in from community members to put new facilities in their neighborhoods. As a result of all these hurdles, she said, “The number of providers that do that type of care is rather limited.”
State regulations require that people who qualify for special treatment services should not be in regular nursing homes; yet CDPH told us that since 2012, they’ve only cited one facility for violating that rule.
Our data could not help us determine how many California nursing home residents need STP services.
We asked CDPH how many residents with serious mental illness need STP services but are not getting them; a spokesperson for the agency said it did not have this information.
Tony Chicotel, with California Advocates for Nursing Home Reform, is not surprised. He said CDPH’s lack of information is consistent with the “hands-off policy” of mental health regulation in nursing homes. “To me, the spirit of the law and the [regulations] are clear,” he said. “Nursing home residents with mental health problems should get special services to treat those mental health problems. And I think what we’re seeing is the system is not addressing those needs.”

How citations fall short
While the state doesn’t keep tabs on exactly how many residents with serious mental illness are in a particular nursing home, they do respond to complaints and check on facilities during the re-licensing or re-certification process. In their joint email, the agencies told us, “If facilities are found to be out of compliance with requirements, CDPH takes enforcement action within its authority.”
Typically that means issuing citations and fines. For example, Hyde Park Healthcare Center, where Travell Jackson worked, has been cited 16 times by DHCS since 2016 for “A-level” infractions—violations that caused an “imminent danger” or “substantial probability of death or serious harm to patients.”
According to one citation, the facility failed to monitor the whereabouts of a suicidal resident with schizophrenia for 32 days.
According to another, a resident with schizophrenia “elope[d] from the facility undetected” and was missing for 23 consecutive days before being found 18 miles away in a vegetative state with blunt-force head trauma.
In yet another citation, Hyde Park employees failed to supervise a resident with schizophrenia who attacked two other residents and staff members, sending one person to the emergency room.
Hyde Park was fined a total of $280,000 during that seven-year period, but has been allowed to operate.
The number of residents with serious mental illness at Hyde Park, coupled with the lack of training, “created an unsafe environment,” said Danielle Sharber, another former employee. “It’s dangerous and unfair.”
Until this past June, Hyde Park was owned by ReNew Health, which LAist wrote about in 2021; ReNew still helps operate the facility, according to Dan Kramer, a spokesperson for the company. Kramer said ReNew’s “principal focus is and will continue to be, providing the best patient-driven health care, and providing a safe environment for our patients and staff.”
Dozens of other facilities are also regularly cited and fined for equally severe infractions. Our investigation found that facilities with a high number of residents who have serious mental illness are on average cited more often than facilities that have fewer residents with serious mental illness.
Charlene Harrington, the professor of nursing at UCSF, said that rather than just hit these facilities with fines when something goes wrong, state regulators should pay closer attention to nursing homes that have a high number of residents with serious mental illness and take more meaningful action.
The state “should be investigating,” she said, “because [nursing homes] certainly shouldn't have that large of a population unless they’re a special treatment facility.”
Can Newsom’s new mental health plan help?
In March, California Gov. Gavin Newsom stood before a podium inside a hospital in San Diego, flanked by local and state officials, to speak about the state’s ballooning homelessness and mental health crises. The state’s lack of housing for people with mental illness and substance abuse disorders are “the most acute challenge the state faces,” he said.
Moments later, Newsom unveiled a new “mental health housing” plan. Endorsed by the National Alliance on Mental Illness California, business groups and city governments, the plan has two parts, one of which would put a decision before voters in March 2024 for a bond measure to create 10,000 new “behavioral health” beds. (A 2021 study by the RAND Group estimated the state was short about 7,700 psychiatric beds.) The plan also calls for funds from a millionaire tax for mental health services to be used for housing programs for people who are unhoused or living in tent encampments.

The governor’s proposal comes just a year after he introduced another sweeping plan, called CARE Court, which is meant to compel people with untreated, serious mental illness into treatment.
His new plan called for building more “campus-style” facilities and other residential settings staffed with mental health services. A press release later described them as “unlocked, community settings.” Newsom made clear they would not be “institutions of the past, but locations where people can really heal.”
Disability and civil rights advocates are skeptical. “There wasn’t a lot of talk about recovery, about people having careers, about people kind of building their lives back. There was talk about beds — ‘We need more beds’ — and I just think that’s a dangerous way to frame it,” said Andy Imparato, executive director of Disability Rights California, who lives with bipolar disorder. “It's like, ‘Let’s find places for these people to go so we don’t have to look at them on the street.’”
Last week, lawmakers added an 11th-hour amendment to the bond measure that alarmed advocates. The addition removed language that the money must be used toward “voluntary, unlocked” settings. The measure passed the legislature overwhelmingly.
Rachel Bhagwat, legislative advocate with ACLU California Action, called the last-minute maneuver a “red flag.”
“There’s a concern that California may be funneling funds toward more institutional settings at the expense of investing funds in less restrictive levels of care,” she said.
We shared our nursing home findings with the governor’s office and asked them to comment about concerns that Newsom’s new mental health plan could lead to more people being institutionalized. The governor’s office forwarded our email to the Department of Health Care Services. “This characterization is inaccurate,” wrote DHCS’s Anthony Cava. “The measure will fund the entire range of treatment sites, residential care settings, and supportive housing.”
He noted that the “Governor’s plan is specifically aimed at people with serious mental illness… to provide the treatment and housing that best suits the individual.”
Imparato, with Disability Rights California, said he agrees that everyone needs housing, but “beds” — like those in nursing homes — aren’t the best placement for people with serious mental health conditions.
“If the best we can do is just find somebody a bed in a place where they’re gonna be isolated, not have much of a life, not have much connection to their family or friends, not be able to hold down a job,” he said, “that’s not a great goal for public policy for people with long-term disabilities.”
Listen
Elly Yu and Elisabeth Gawthrop joined LAist 89.3's AirTalk show on Sept. 20 to discuss their findings and take listener calls. Also appearing: Rachel Tate, vice president of Ombudsman Services at WISE & Healthy Aging, and Tony Chicotel, senior staff attorney at California Advocates for Nursing Home Reform.
Mental health resources
-
- Steinberg Institute website, links to mental health resources and care throughout California
-
- Institute on Aging's 24/7 Friendship Line (especially for people who have disabilities or are over 60), 1-800-971-0016 or call 415-750-4138 to volunteer.
-
- Los Angeles County Department of Mental Health, 24/7 Access Line 1-800-854-7771.
-
- The Crisis Text Line, Text "HOME" (741-741) to reach a trained crisis counselor.
-
- California Psychological Association Find a Psychologist Locator
-
- Psychology Today guide to therapist
-
If You Need Immediate Help
-
- If you or someone you know is in crisis and need immediate help, call the Suicide Prevention Lifeline at 988 or go here for online chat.
-
More Guidance
-
- Find 5 Action Steps for helping someone who may be suicidal, from the National Suicide Prevention Lifeline.
-
- Six questions to ask to help assess the severity of someone's suicide risk, from the Columbia Lighthouse Project.
-
- To prevent a future crisis, here's how to help someone make a safety plan.
-
This story is a collaboration between LAist, APM Research Lab and The California Newsroom (a collaboration of public media news outlets throughout the state).
-
More on the team behind this investigation:
-
LAist
- Elly Yu, Investigative Reporter
- Megan Garvey, Executive Editor
- Brian Frank, Editor, Digital and Special Projects
- Dan Carino, Senior Designer (illustrations)
- Samanta Helou Hernandez, Visual Journalist (photos)
- Kristine Malicse, Social Media Producer
- David Rodriguez, Partnership Producer
-
APM Research Lab
- Elisabeth Gawthrop, Data Journalist
- Craig Helmstetter, Managing Partner
-
The California Newsroom
- Mike Kessler, Investigations Editor
- Adriene Hill, Managing Editor
- Emily Zentner, Investigative Data Journalist
-
Additional assistance
- Sherri Hildebrandt, Copy Editor
-
Note: Kessler served as the main story editor and Hill edited the audio reporting.
-
The Jane and Ron Olson Center for Investigative Reporting helped make this project possible. Ron Olson is an honorary trustee of Southern California Public Radio. The Olsons do not have any editorial input on the stories we cover.
-
The project was also supported by the Carter Center’s Rosalynn Carter Fellowships for Mental Health Journalism.







