On May 11, the U.S. COVID-19 public health emergency expires. A separate national emergency was also set to expire, but was rescinded early by President Biden.
Local public health emergencies in California and Los Angeles County have already been rolled back.
What changes when the public health emergency ends?
Congress has denied the Biden administration's requests to fund more COVID tests and vaccines, so the portion that affects most Americans has already been curtailed. When existing supplies already paid for with federal dollars run out they will not be replaced.
Treatments and vaccines still free
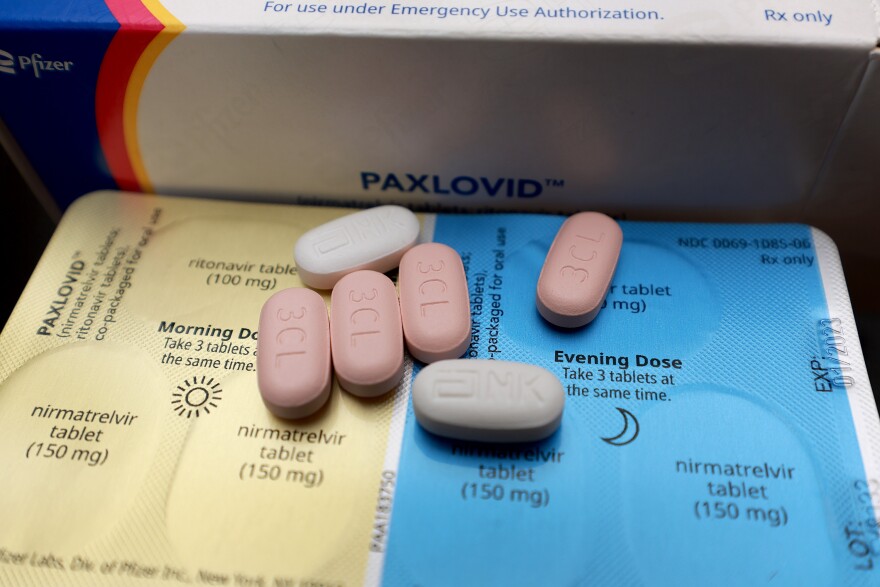
If you test positive for COVID after May 11, you’ll still be able to get free treatments such as Paxlovid as long as the federal government’s supply lasts. After that, it depends on which state you live in.
-
What candidates can — and can't — say they do
-
Nonprofit's launching fundraiser to keep it afloat
-
USC study documents what residents want from trees
Most health plans in California will continue to cover treatments until Nov. 11 (more on that below) while those with Medicare will face out of pocket costs, depending on their health plan. How much you’ll pay for antivirals will depend on what type of health insurance coverage you have.
COVID vaccines will still be free. The Centers for Disease Control and Prevention recommends that everyone 6 months and older receive the bivalent vaccine, which protects against circulating omicron variants. People 65 and older and those with compromised immune systems can get a second dose.
Why California is different
State lawmakers effectively added six months to the federal public health emergency. That means health plans regulated by the California Department of Managed Health Care are required to continue to pay for COVID tests, vaccines, and treatment, both in and out of network without prior authorization or cost-sharing.
Enrollee cost-sharing includes co-pays, co-insurance, deductibles or other enrollee out-of-pocket costs not including health plan premiums. This includes health coverage many get from their employers, as well as plans managed by Medi-Cal and Covered California. After it expires Nov. 11, most insured people in California will only have cost-sharing if those services are provided out of network.
What about other health plans?
Some health plans aren’t managed by DMHC, such as Medicare. For Medicare Advantage members in California starting on May 12, 2023:
- COVID vaccines will continue to be covered at no cost.
- COVID PCR testing (which requires a specimen or swab be sent to a lab) will be covered but you’ll pay out-of-pocket costs. The amount depends on your plan.
- At home COVID test coverage expires and will no longer be covered.
- COVID treatment will be covered with applicable plan out-of-pocket costs.
- Any COVID related out-of-network services such as testing, vaccines, and treatment will only be covered in emergency or urgent care situations or when out-of-network coverage is included in your plan.
I live in California. What should I do if I receive a charge or bill for a COVID-19 test, vaccine or treatment?
Here’s the advice from the California Department of Public Health:
If you have health coverage through a health plan and receive a charge or bill related to the coverage or administration of a qualifying COVID-19 test, vaccine or treatment, you should first contact your health plan to file a grievance, sometimes called an appeal, and include a copy of the bill. The health plan will review the grievance and should ensure you are not charged or are reimbursed if you already paid a bill.
If you do not agree with your health plan’s response or if the plan takes more than 30 days to fix the problem, you should contact the DMHC Help Center or call 1-888-466-2219.